Social work is a field in which professionals are intended to do their best to help connect members of vulnerable populations with the resources necessary to allow them to live with their rights and general well-being safe. However, on October 12 of this year, during a meeting between the Texas Behavioral Health Executive Council and the Texas Board of Social Work Examiners, a section of the social workers’ code of conduct was altered. A section which previously stated, “A social worker shall not refuse to perform any act or service for which the person is licensed solely on the basis of a client’s age; gender; race; color; religion; national origin; disability; sexual orientation; gender identity and expression; or political affiliation.” During the meeting, the words “disability; sexual orientation; gender identity and expression” were taken out. They instead replaced that phrase with the word sex, making the social workers’ code match the Texas Occupations Code.
This is concerning for a few reasons, the most glaring one being that it leaves members of the LGBTQ+ community and people with disabilities in Texas, two populations that are already seriously vulnerable, even more vulnerable than before, as social workers can now turn away potential clients from those communities.
This led to an uproar among advocates for the LGBTQ+ community and people with disabilities, as at puts their ability to access important resources that are related to their basic human rights directly at risk. There is an increasingly serious concern that members of these populations will face even more obstacles in accessing the things they need than they already do.
The Human Rights Connection
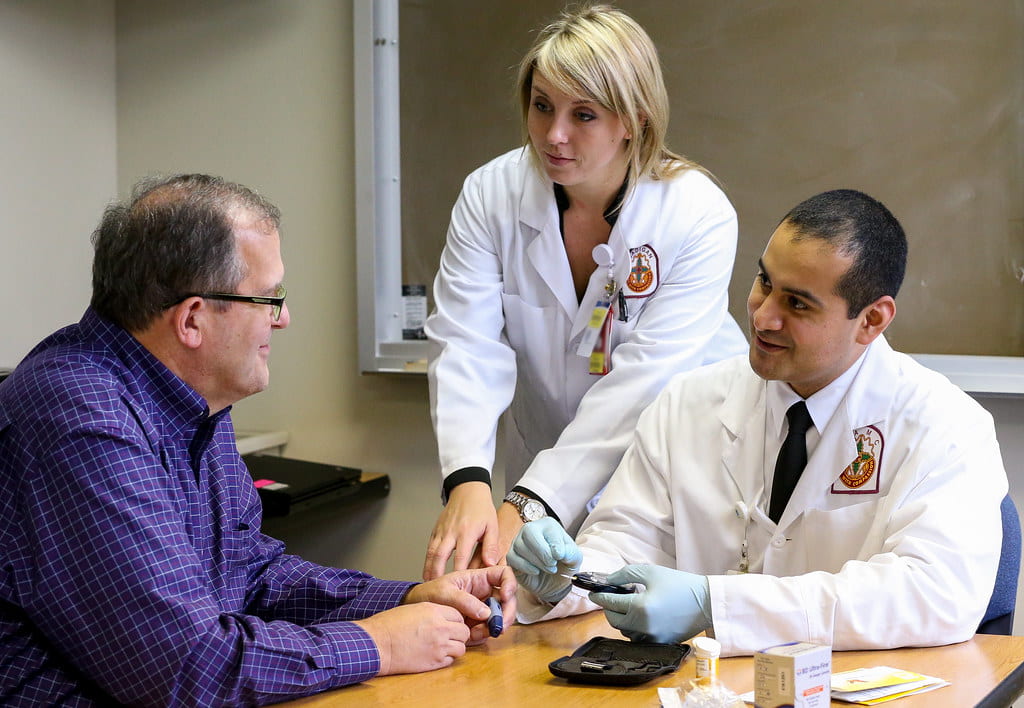
It’s important to recognize that is an issue of human rights, even outside of the clear issue of discrimination against these groups that is involved. Consider some of the jobs of social workers. They include therapists, case workers, workers for Child Protective Services, and much more. In addition to working with people with disabilities and members of the LGBTQ+ community in general, many social workers specialize in work with children and older adults, two groups which overlap with the former. Then these vulnerable populations are unable to get the support they need in order to access the tools, programs, and resources that exist specifically to help them live life and access their basic needs, they are by extension often kept from being able to access their basic human rights.

One clear example of this is when people with disabilities require financial aid to support themselves do to an inability to be a part of the general workforce. Social workers are an important part of the process of connect the people affected by this issue with the resources and government programs they need. Without the aid of social workers, they might have significant difficulty accessing their “right to a standard of living adequate for the health and well-being of himself and of his family, including food, clothing, housing and medical care and necessary social services, and the right to security in the event of unemployment, sickness, disability, widowhood, old age or other lack of livelihood in circumstances beyond his control,” as recognized in Article 25 of the United Nations’ Universal Declaration of Human Rights.
The fact that this allows social workers to discriminate certain groups in accepting clients is human rights issue in itself, as according to Article 7 of the UDHR, all are entitled to equal protection under the law and, “All are entitled to equal protection against any discrimination in violation of this Declaration and against any incitement to such discrimination.”
The Purpose of Social Work: Helping Vulnerable Populations
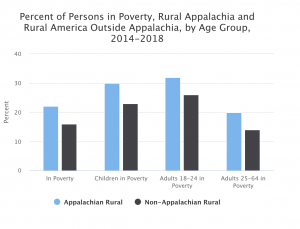
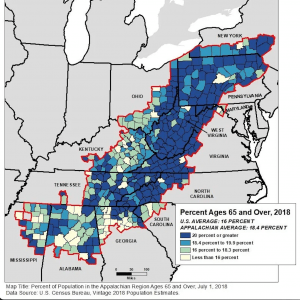
Another reason this change in the Texas social workers’ code of conduct is problematic is that the field of social work is inherently meant to involve professionals helping vulnerable populations (such as the LGBTQ+ community and people with disabilities). According to the National Association of Social Workers’ (NASW) Code of Ethics, “The primary mission of the social work profession is to enhance human well–being and help meet the basic human needs of all people, with particular attention to the needs and empowerment of people who are vulnerable, oppressed, and living in poverty.” A vulnerable population is a group or community “at a higher risk for poor health as a result of the barriers they experience to social, economic, political and environmental resources, as well as limitations due to illness or disability.”
Social work is also built a set of core values: service, social justice, dignity and worth of the person, importance of human relationships, integrity, competence. It is the job of a social worker to do what they can to uphold those values by helping vulnerable populations access the resources they need. Therefore, social workers’ turning away members of the LGBTQ+ community and people with disabilities, particularly vulnerable groups, goes against the social work code of ethics.
The ethical principles of social work also bar social workers from participating in acts of discrimination on the “basis of race, ethnicity, national origin, color, sex, sexual orientation, gender identity or expression, age, marital status, political belief, religion, immigration status, or mental or physical ability.”
There is a meeting set for October 27, 2020 so that the Texas Behavioral Health Executive Council can discuss the issue of discrimination as it applies to the changes that were made to the Texas social workers’ code of conduct. It is vital that we do not underestimate the significance of this situation and the serious harm that it can cause.