What Is a Food Desert?
Source: Mike Mozart via Flikr
Currently in America, the neighborhood you were born in can affect your future income, education level, and your ability to consistently access nutritional food. The Food Empowerment Project (FEP) defines food deserts as “geographic areas where residents’ access to affordable, healthy food options (especially fresh fruits and vegetables) is restricted or nonexistent due to the absence of grocery stores within convenient traveling distance”. The USDA has defined two types of food deserts: one that exists in both rural areas more than 10 miles from the nearest store and the second which exists in urban environments, where citizens face daily obstacles in obtaining healthy food due to lack of availability or resources. But, the average conversation about food deserts surrounds zones within American cities where citizens, hindered by lack of access to transportation and restricted budgets, are unable to obtain nutritional food. Food deserts play a critical role in food insecurity in the United States, and they are typically visible in urban areas where the residents are already living in extreme economic hardship.
The Institute of Human Rights at UAB has recently published an article about food deserts in our hometown of Birmingham, Alabama that you can read here– but for readers in other parts of America, I want you to do an exercise with me. Think about your nearest big city, or an urban area you are familiar with. This can be in New York City, Atlanta, Miami, Chicago, or whichever metropolis best applies to you. Visualize the roads you drive, the areas both wealthy and impoverished. Now, think of the few streets within that city where there are almost no Walmarts, Targets, Krogers or Publix chains. In this stretch, there are tons of fast food restaurants, cash bond and payday loan businesses, laundromats and gas stations. There is an abundance of drive throughs and minimarts, but you could drive for a few minutes before you find a grocery store. Can you see that part of your city in your head now? THAT, dear reader, is your local food desert.
Note: The USDA compiled census and other data into an interactive map called the Food Environment Atlas, which allows any user to view rates of food insecurity, diet quality, and food prices in your area or any neighborhood you are curious about. If you struggle to think of a food desert near you, or want to learn about what areas are impacted by food insecurity, I recommend you try out the Food Environment Atlas here.

The Cause:
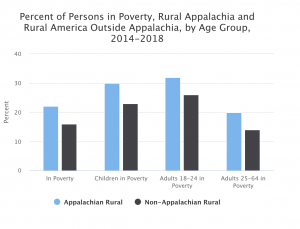
Food Deserts have typically been attributed to socioeconomic status. One of the main characteristics that defines a food desert is lack of accessibility, which means people living in a certain region have limited resources, be it money, time or transportation to access nutritional, fresh food. Food deserts are most common in low socio-economic areas, where residents are unlikely to own a car or have one that is not always working. Americans living here typically live paycheck-to-paycheck, and require both accessibility and affordability to make ends meet throughout the month. It is currently estimated that one in six Americans still experience food insecurity, and that roughly 19 million people are affected by food deserts or limited access to supermarkets in America. Recent studies by the United States Department of Agriculture confirm the connection between race and food deserts, stating in 2019 that “rates of food insecurity were substantially higher than the national average for single-parent households, and for Black and Hispanic households”.
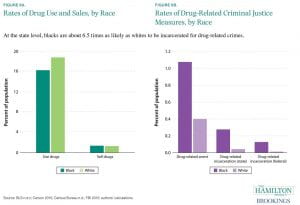
The conversation surrounding food deserts has shifted to include race in recent years. Originally, the term food desert was coined to represent the socioeconomic disparities that cause some Americans to face food insecurity. Now, organizations like the Natural Resources Defense Council (NRDC) are pushing to recoin the term as food apartheid to accurately represent the way food insecurity affects those of minority race in America. The NRDC explains the term shift, saying that,
“Many groups are now using the term “food apartheid” to correctly highlight the how racist policies shaped these areas and led to limited access to healthy food. Apartheid is a system of institutional racial segregation and discrimination, and these areas are food apartheids because they too are created by racially discriminatory policies. Using the term “apartheid” focuses our examination on the intersectional root causes that created low-income and low food access areas”.
Essentially, it is vital that we recognize how a historical and current racial inequalities act as a cause of both the food deserts and the zones of poverty they’re found in. The historically black areas of segregated cities were underfunded and underdeveloped, plagued by lack of opportunity and equal access, and in some areas across the United States an economic shadow of that segregation still remains.

Their Effect and Why It Matters:
America has incredibly high rates of obesity and nutrition-based health issues in comparison to other developed countries. While there are decades of research connecting poverty and race to higher rates of nutrition-based disease and other health issues in America, science is now beginning to track the specific effects of food deserts on obesity and chronic illness. A corner store or a pocket-sized version of big supermarket chains like a Walmart Neighborhood Market, but if you take the time to walk inside you’ll see the fresh produce section is either neglected or nonexistent. These smaller stores have less room for inventory, their foods are less likely to be fresh produce due to the requirements to keep them fresh, and these foods are often packaged and processed. That means those who depend on these stores are limited to fast food, packaged goods, or other processed and low quality options that can contribute to malnutrition, heart disease, obesity, diabetes and more.
In addition to the effects of food deserts on health, the prices per unit are almost always more expensive than their suburban, chain-grocery counterparts. A person who can afford a Costco membership will almost always spend less on the same food products as a family living paycheck to paycheck or utilizing EBT for groceries. A 1997 USDA study found that “geographic location was the single most important contribution to higher nationwide average prices faced by low-income households”, and that smaller stores charged more per item than supermarkets nationwide. Food scarcity and cost disparities disproportionately affect minorities and those already living in financial insecurity, and each city has a part to play in ending this national crisis of inequality.

Join the movement to end food insecurity in the US:
Ultimately, the end to food desertification requires an effort between elected officials and businesses to make nutritious food affordable and accessible for all people. If you recognized a food desert near you in the imaginative exercise we did earlier, that could be the perfect topic to address with your local lawmakers through emails, calls or petitioning. If you prefer other types of action, there are countless ways to work as individuals to help your community in the meantime. Getting involved in the fight against food insecurity can be as hands-on and involved as you want, from donating non-perishable foods and needed items to local organizations, shelters or food kitchens to establishing a community garden, or everything in between. There are plenty of ways to make a difference at whatever level of involvement works best for you, and I’ve linked some of my favorites below!
A Few Ways to Get Involved:
- Click HERE to find your elected officials on the state and local level and how to contact them about the food deserts affecting their voters. You can use your voice to push for changes that directly impact your community in a positive way.
- Feeding America is a charity that uses your donations to help the 1 in 8 Americans experiencing hunger now. This link takes you straight to their front page, which features a zip code locator for the closest food bank to you!
- Organize or contribute to a local food drive. Many public schools and local businesses run food drives for charities throughout the year, and Rotary International has an awesome guide available for starting your own community food drive HERE. Sharing surplus food is an excellent way to help others while reducing waste as well!
- Use this link to find food pantries near you to donate, volunteer, and get involved in your state’s fight against food insecurity.
- Find what works for you. Try searching for more ways to get involved that are tailored to your area and preferences…every contribution helps!