Everyone has heard of global poverty and its horrendous consequences; however, for some people, that is where their knowledge ends. In this blog, I am going to undertake the task of succinctly compiling facts and statistics about this incredibly broad topic. My hope is that, after reading this blog, you are more inclined to speak out on global poverty and educate others on the topic.
A Rudimentary Understanding

Global poverty is an umbrella term for poverty that exists throughout the entire world. That was the easy part: defining global poverty. However, defining poverty is a tad bit more tricky. We can surely say that poverty is a status: the status given to those whose annual income falls under a bar; however, poverty is more than just low annual income.
The United Nations, in particular, has defined poverty as, “a denial of choices and opportunities, a violation of human dignity. It means a lack of basic capacity to participate effectively in society. It means not having enough to feed and clothe a family, not having a school or clinic to go to, not having the land on which to grow one’s food or a job to earn one’s living, not having access to credit. It means insecurity, powerlessness, and exclusion of individuals, households, and communities. It means susceptibility to violence, and it often implies living in marginal or fragile environments, without access to clean water or sanitation.”
In addition, when discussing poverty, there is a distinction between relative deprivation and absolute deprivation. Relative deprivation is a function of inequality and can be defined as “the lack of resources (e.g. money, rights, social equality) necessary to maintain the quality of life considered typical within a given socioeconomic group.”
Absolute deprivation, on the other hand, is when one’s income falls below a level where they are unable to maintain food and shelter. Studies have shown that relative deprivation, or the inability to live up to the basic standards of living set forth within a particular community of reference, can be just as harmful to health outcomes as absolute deprivation. For example, research suggests that diabetes – a disease associated with modernization – is not a function of poverty, as the poorest countries show the lowest incidence among the global population. It is in nations that exhibit increasing political-economic and social inequality, including the United States, that diabetes has emerged as a leading cause of death and a serious public health threat.
Therefore, it should go without saying that our goal should be to diminish all forms of deprivation globally.
Statistics and Facts

Personally, what I find most disturbing about global poverty is its breadth. Grounding this point is the fact that, according to the World Bank and WorldVision, “About 9.2% of the world, or 689 million people, live in extreme poverty on less than $1.90 a day.”
Practically one in ten people within the world are living in poverty.
To better understand the magnitude of this issue, imagine the following scenario: you live in this fantasy world where, in an effort to promote international toleration and cooperation, 30 children from all around the world get arbitrarily placed together into a classroom. Out of those 30 children, three of them would be living on less than $2 a day. If you are reading this blog, then you naturally have access to some sort of electric device. Those three children, in a year, will not have accumulated enough money to purchase your device.
A logical question that might follow from the preceding scenario is that it is wrong of me to solely include children in made-up scenarios because adults, after all, also live in poverty. While that is undeniably true, they by no means make up the majority. Over two-thirds of those living in poverty are children. Of those children, women represent the majority.
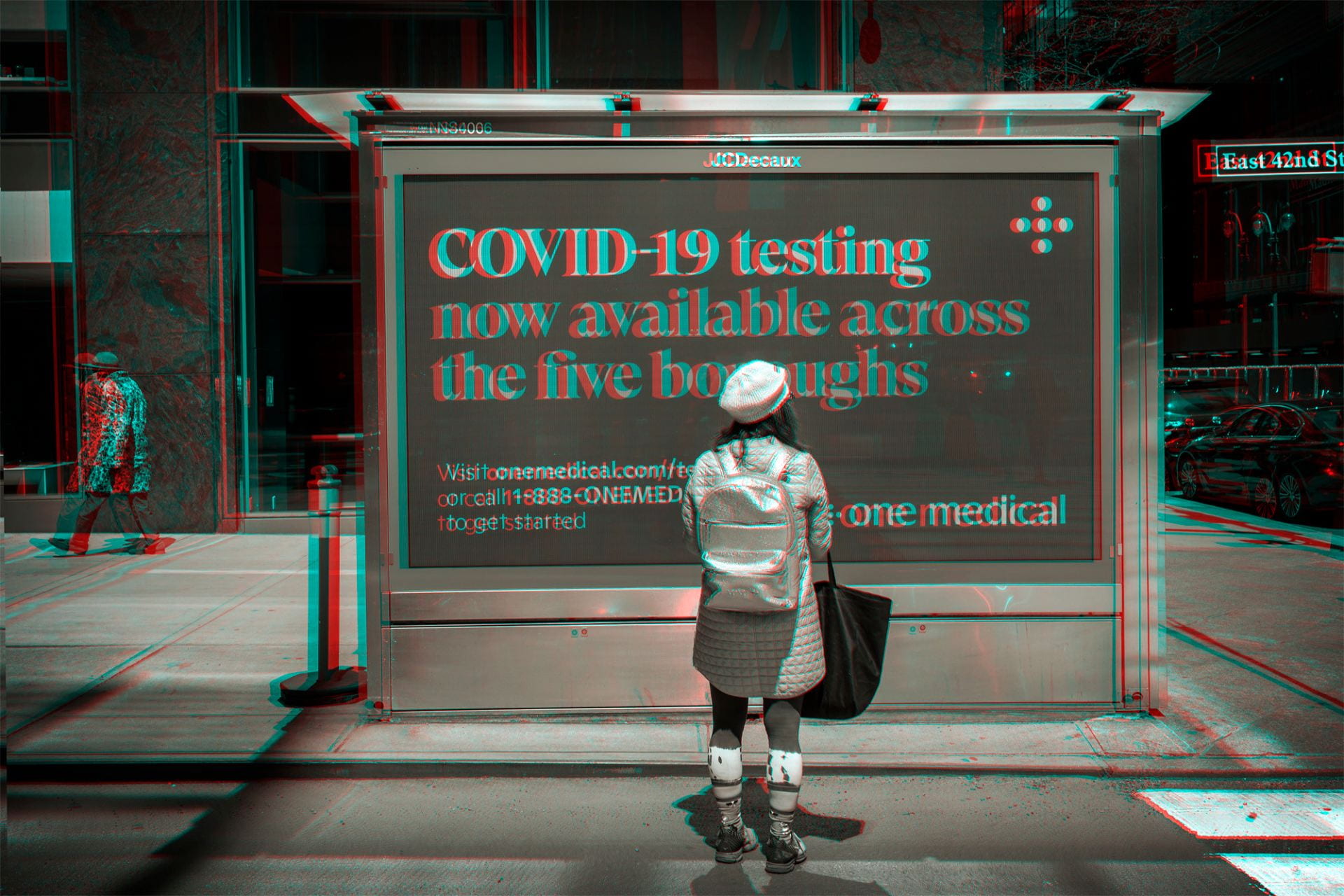
Let us quickly look at local poverty—specifically, poverty within the United States. In the United States, as of 2019, around 10.5% of people live in poverty. The poverty line in the United States is around $13,000, and thus, each person living in poverty makes around $35 a day. Let us make note that these statistics are from 2019, meaning they are pre-pandemic. In 2020, the percentage of people living in poverty went up by one point to 11.4%. Ostensibly, that raise seems miniscule; however, it accounts for 3 million new Americans who entered poverty, also now making less than $35 a day.
All poverty is bad: that is undisputed. However, one who lives in America might confuse American poverty with global poverty as it might be what they encounter daily. This presents a problem because this cannot be done as they are by no means the same. Those in poverty in America statistically make ten times more a day than those living in poverty abroad. That is a big difference; we can not equate the two.
Education

Education is a human right; that is undeniable. Every human who walks this Earth has the right to get an education and develop individually. However, living in poverty makes education incredibly difficult.
One study has found that, of those who live in poverty and are over the age of 15, 70% have only a basic education with no formal schooling. That means that if you are born into poverty and have no way of elevating out of this status, then, statistically, you are unlikely to get an education. This is an immense issue due to the fact that, according to UNESCO, education is the key to climbing out of poverty. In fact, UNESCO stated that, “if all students in low-income countries had just basic reading skills (nothing else), an estimated 171 million people could escape extreme poverty. If all adults completed secondary education, we could cut the global poverty rate by more than half.”
The dilemma is that the path out of poverty is through education; however, living in poverty makes education harder to achieve.
However, in the past years, steps have been made in the correct direction, and education rates have indeed increased. A rise in education is beneficial to not just those living in poverty, but the nations they live in as well. In fact, a study published by Stanford University and Munich’s Ludwig Maximilian University shows that, between 1975 and 2000, 75% of the increase in a nation’s gross domestic product (GDP) can be attributed to the increase of math and science skills amongst the population.
Therefore, education not only improves the lives of those in poverty, but also the well-being and economy of the nation and its people. It is for those reasons, amongst many more, that education is, and should forever remain, a human right.
Impacts

In addition to the lack of education, those living in poverty face a multitude of other negatives. For one, a study found that adults living in poverty are at a “higher risk of adverse health effects from obesity, smoking, substance use, and chronic stress. [IN ADDITION], older adults with lower incomes experience higher rates of disability and mortality.”
In addition, this same study found that those living in the top 1% generally have a life expectancy 10 years greater than those living in poverty. Moreover, one study found that, for children and adolescents, poverty can also cause differences in structural and functional brain development, which impacts “cognitive processes that are critical for learning, communication, and academic achievement, including social emotional processing, memory, language, and executive functioning.”
Therefore, with the aforementioned facts in mind, it is easily concluded that poverty is an immense issue, and political leaders should be doing more to help relieve the issue.
So, naturally, one might ask: why is nothing being done? One response to this question comes from the World Systems Theory. This theory is complex, so I will try my best to briefly discuss it. The theory states that all nations are divided into three systems: the core, the periphery, and the semi-periphery. Essentially, the theory states that the core nations, which are the most politically and economically powerful, use the periphery and semi-periphery nations, which are filled with developing nations, for cheap labor and resources. The core rewards the periphery for their resources and labor, but not enough that the nations develop at such a pace that they become equal to the core nations. This in turn causes a dilemma in which the periphery depend more on the core than vice versa. Some might argue that this in turn perpetuates global poverty as the core nations are doing the least to help developing nations. In other words, the rich get richer and the poor get poorer, thus exacerbating both absolute and relative forms of deprivation and sustaining the cycle of poverty.
Moving Forward

As mentioned previously, global poverty has indeed been decreasing. According to WorldVision, “Since 1990, more than 1.2 billion people have risen out of extreme poverty. Now, 9.2% of the world survives on less than $1.90 a day, compared to nearly 36% in 1990.”
We are still heading down this path of poverty reduction, and it is vital that we continue to do so. Perhaps, one day, we will live in a world free of poverty—a world in which every single person is educated, well-nourished, and does not have to fear starvation. It is my hope that after you finish reading this blog, you will share any knowledge and statistics you may have learned with others. The first step in resolving an issue–and continuing to resolve it—is acknowledgement. If more people are aware of how detrimental poverty is, more people will in turn be inclined to help fix it. We need more support and commitment to a world in which poverty is mere history.