Humans have always been regarded as higher animals due to several similarities we share, including instinct, cognition, problem solving skills, introspection, creativity, emotional intelligence and planning skills. Just as planning is an ability of both humans and animals, it involves adequate effort and encompasses a wide range of ideas and research put in place to actualize our desired objective. One of the most fascinating parts of planning to me includes identifying the best place or location we can truly reach our goals, achieve our objectives and fulfil our purpose, which all basically centers around migration. Migration remains a constant and unending phenomenon for both humans and animals, and various motives can be attributed to this endeavor, such as the search for food and water, seasonal weather change, mating reasons, employment opportunities, health and education reasons, adventures and thrills, insecurity, and many others. More still, we can basically summarize migration purposes as a search for a better life, which is a basic instinct all living things possess.
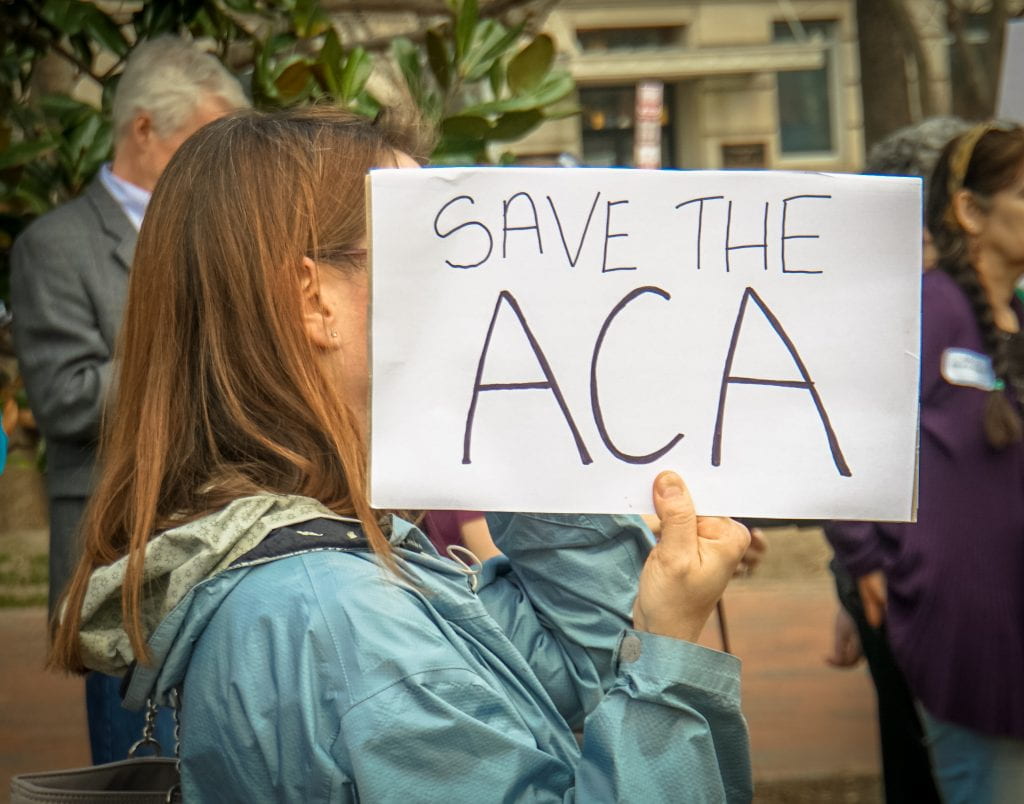
In the last ten years, migration within the international context has risen to a significant level despite continuous efforts many countries have dedicated in ensuring their borders are adequately tightened with hope of discouraging immigrants from illegally entering their borders. According to Ross, Cunningham, & Hanna, an estimation of 244 million migrants are presently living temporarily or permanently outside their country of birth. Violent conflict, discrimination and lack of employment opportunities are major reasons for the increasing number of immigrants in several developed countries, and has forced many countries into adopting drastic measures such as rigorous identity checks, detention camps and deportation, to reduce their entry. Another means of curbing the increasing number of immigrants includes formulating and enforcing policies that limits them access to affordable healthcare services. For instance, the United States Affordable Care Act excludes undocumented immigrants from accessing health insurance, while the immigrant provisions of the 1996 Welfare Reform Act, the Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA) excludes undocumented immigrants from publicly funded services.
Several immigration laws and policies within the United States continuously hinder undocumented immigrants’ access to adequate healthcare services, which constitutes a major challenge to all who fall under this category despite evidence proving they contribute more money in taxes to the U.S. economy than they consume in services. What I believe the U.S. government has failed to understand is the fact that these laws and policies not only put the health of these undocumented immigrants at a high risk, but also the health of the general public and socioeconomic development of the country. One of the most detrimental ways these laws and policies have greatly affected this vulnerable population is in the fight against the HIV epidemic. According to Ross et al., migrants who reside in developed countries are disproportionately affected by HIV as the proportion of new HIV diagnosis amongst migrants exceeds the percentage of the general population. HIV, as we all know, is a global epidemic that demands the best care and treatment which was the reason that spurred world leaders in 2015 to restate their commitment to the right to health by enacting the universal health coverage in the sustainable development goals that guarantees all people and communities access to high quality health services.

It is clear the United States government clearly disregards this universal policy that aims at ensuring everyone receives the best healthcare services irrespective of their personality or condition. I guess the U.S. government by their own understanding believes migrants do not fall under the universal coverage as it is evident through their discouraging treatment of undocumented immigrants, more so, those living with HIV. Ross et al. believes migrants persons living with HIV have more characteristics that are associated with poor HIV clinical outcome, and are more likely to die from HIV compared to non-immigrants. For undocumented people living with HIV, there are more factors that exacerbate their condition such as discriminatory laws and policies, lack of follow-up care, ignorance, stigmatization and discrimination. I do believe these discriminating laws and policies serves as the major factor affecting undocumented people living with HIV. One area that typifies this can be seen during the documentation process of a patient health record, which compulsorily demands the immigration status information of individuals. This got me wondering if a client’s immigration status information is actually needed in their health record.
Kim, Molina & Saadi believes documenting immigration status in patient records not only possess a challenge to the clients but also to clinicians. Although by recording this, the information would most likely improve the communication process between the client and the clinician, and also facilitate continuity of care, on the other hand, recording the same information could expose the client alongside their family to risks of being stigmatized or discriminated by non-immigrant friendly clinicians who may expose them to immigration enforcement officers even though it violates patient confidentiality. They believe explicit documentation of immigration status of patients alongside their families in a health record be avoided as evidence suggest risks outweigh benefits in this regard. Conversation about immigration status using indirect language in describing social context should rather be prioritized over written documentation to ensure patients have their healthcare needs met without fear. They concluded by advising clinicians and the general healthcare system to ensure policies and guidelines reduce the high level of stigma and discrimination for all rather than the present opposite.

Another area that strikes me hard for undocumented immigrants living with HIV are those who are currently in detention camps across various states in the U.S., a revelation which came to me through one of my on-campus events with the representative of the Alabama Latino Aids Coalition. The speaker spoke about the inhumane treatment undocumented immigrants go through while in detention, more so, people living with HIV. This made me do some research and I found several evidences that confirmed undocumented immigrants living with HIV can actually maintain continuous access to care and treatment while being detained in correctional facilities to ensure they sustain or achieve good virologic outcomes and well-tolerated regimens if structured protocols are implemented and enforced. It should be noted that the detention process for migrants during their deportation proceedings is complex and rigid which has led to several lapses due to poor access to proper medical care. Even though there are 21 Federal Detention Centers across the U.S., which are operated by the Bureau of Prisons, and all provide Antiretroviral treatment and medication to detainees who disclose their HIV status, there exists fear of stigmatization or discrimination amongst detainees living with HIV as they believe their disclosure may negatively impact their immigration trial, especially if they also fall under any gender or sexual minority groups. Also, the poor living condition and environment of this population while in detention forces some to relapse into substance use, engage in risky sexual behaviors, and disregard their treatment plan.
Based on this understanding, it is hard to imagine the inhumane condition undocumented immigrants are forced to live through while being detained. There is need for the U.S. government to understand that even though several undocumented immigrants after their trial, are usually deported or released at the nearest borders or territories close to their home countries, several others return into the society without receiving adequate rehabilitation or reintegrative education which possess a challenge to the society at large. Human and material resources that could have been used to resolve other pressing needs will then be used to serve their avoidable demands. To resolve this challenge, there is the need to abolish any form of discrimination against detainees living with HIV and ensure it does not affect their deportation trial. Also, clinicians and correctional officers need to be more sensitive to the needs of the detainees having been separated from their families and may never see them again, which is a situation that can easily exacerbate their condition in such a hostile detention environment. Human rights institutions, immigration right advocates, academicians, alongside health authorities, media and the general public should also advocate and help raise awareness about the poor condition of these detention facilities. For deported detainees living with HIV, the U.S. government alongside non-governmental institutions should provide adequate health education using evidence-based treatment medications and materials that meets the specification of their home country to ensure transnational HIV continuity of care.

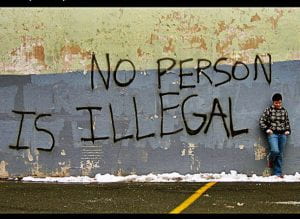
In all, we all should understand that undocumented immigrants are also humans and should be treated with utmost respect irrespective of their situation. There is need to ensure their health and wellbeing are adequately met and well taken care of. As humans, we should not only sympathize with them, but also support them by raising awareness and advocating for better laws and policies that can assist them during their ordeal. We should always aim for a multi-sectoral approach that addresses the structural challenges for undocumented immigrants living with HIV such as housing, food security, mental health, and access to employment because there is a continuous effort by the U.S. government to dehumanize undocumented immigrants as community members and remove vital resources that is available to them. As we all know the U.S. government remains extremely resolute in enforcing the 2015 immigration laws that places all undocumented immigrants at risk of being deported, they can also ensure the universal law on respect to all life is adequately respected by enforcing laws, guidelines and policies that protects the lives and wellbeing of undocumented immigrants.