December 3rd marked the International Day of Persons with Disabilities – a day to raise awareness of disability rights, the benefits of inclusion, and the challenges society poses for individuals with disabilities. The theme for this year is “Leadership and participation of persons with disabilities toward an inclusive, accessible and sustainable post-COVID-19 world.” In honor of this occasion, we wanted to highlight a few of the many instances in recent times where strides have been made in inclusion and accessibility. This post will focus on the progress made in south Asia, while the post by Danah Dib will speak to the achievements that have been made in the Middle East. There have been numerous successes in the efforts to push disability rights forward in south Asia, particularly in the spheres of politics, health, and education.
Political Rights
Efforts to secure the political and civil rights of individuals with disabilities in south Asia passed a milestone in 2015. The “South Asia Regional Disability Rights Dialogue on Political Participation” convened for the first time in October of 2015, bringing together over 80 representatives from disabled people’s organizations and election management bodies across south Asia. The conference aimed to advocate for increased access to elections for people with disabilities by providing recommendations to the Forum for South Asian Election Management Bodies (FEMBoSA) during its annual conference. After three days of deliberation and advocacy work, the participants in the South Asia Regional Disability Rights Dialogue on Political Participation produced a nine-point charter on disability inclusion in elections and managed to get the Columbo Resolution modified to include language that was inclusive of people with disability. The Columbo Resolution was the culminating document of the conference, setting forth the Forum’s priorities and commitments for the future. In the same document, FEMBoSA also resolved to develop appropriate standards to ensure that people with disabilities are included in elections.
Numerous changes occurred in the wake of this resolution, in part due to continued advocacy by disabled people’s organizations in implementing the recommendations. Smitha Sadasivan, a member of the Disability Rights Alliance India, described the work of the organization in the implementation process in the state of Tamil Nadu, India: “Persons with intellectual and psychosocial disabilities were enrolled in electoral rolls after the Colombo Declaration”. Numerous additional steps were taken, starting with the appointment of officers specifically responsible for disability inclusion. Electors with disabilities were mapped, and reasonable accommodations were identified. Inclusive voter educational material was developed, and election officers and volunteers were trained on inclusive practices. In 2016, the Election Commission of Sri Lanka included a unit regarding disability in its strategic, four-year plan, with the intent to research barriers to inclusion and increase the participation of people with disabilities. These changes are key steps in ensuring that individuals with disabilities are afforded their civic liberties and can take part in shaping their community.

Rights to Health and Healthcare
A second important development for disability rights takes us from the polling booths to hospital clinics. The impacts of healthcare providers holding negative attitudes towards disability, and a lack of knowledge on appropriate communication, is well documented. It not only impacts the doctor-patient relationship and decreases quality of care, but also results in individuals with disability utilizing healthcare services less frequently. It goes without saying that this contributes to worsened health outcomes for those who are disabled. In recent times, the Medical Council of India has taken steps to bridge this deficiency in clinical care. Starting from August 2019, medical schools in India are required to conduct a month-long training on disability rights that covers culturally appropriate communication and optimum clinical care for people with disabilities. This change came after numerous disability rights advocates, and doctors with disabilities, raised their voice regarding the lack of disability related competencies in the new medical curriculum designed by the Medical Council of India in 2018. Spearheading these efforts was Dr.Satendra Singh of the University College of Medical Science in Delhi University.
Collaborating closely with people with disabilities and educators across the country, Dr.Singh and his colleagues developed 27 disability competencies based on the human rights approach to disability, as enshrined in the UN Convention on Rights of People with Disabilities. While more can be done to make education on disability rights increasingly comprehensive and immersive, such as inclusion of experiential learning where medical students spend time with individuals with disabilities outside of the hospital, these actions are undoubtedly a much-needed step in the right direction. India, like many other countries, also faces challenges in increasing medical student diversity in terms of disability – significant, structural barriers still exist for competent medical school applicants with disabilities. Disability rights advocates like Dr.Singh continue to challenge inaccurate and negative stereotypes regarding the abilities of individuals with disabilities, hoping to further improve medical care and education for people with disabilities.

The Role of Non-Governmental Organizations
Another area of development is the not-for-profit sector, organizations that are working at the grassroot level to offer support to individuals with disabilities and to help implement and further systemic policy changes. An example of such an organization is the Rising Sun Education and Welfare Society in Lahore, Pakistan, which aims to encourage the independence of individuals with disabilities through education and training. One noteworthy aspect of the organization is their training in sports. Sports training is offered as a way to develop capabilities and life skills of individuals with disabilities and to allow them to compete at the highest level in international competitions like the Special Olympics. Over the years, athletes from the organization have won 91 medals in numerous events across the world. The organization also provides vocational training in cooking through their “Special Chef” program – individuals who participated in the program went on to not only work for the Education and Welfare Society, but also join other organizations as chefs and start their own business ventures. Lastly, another crucial role the organization plays is in raising awareness amongst parents regarding the support services available to their children with disabilities. These efforts attempt to combat the stigma surrounding disability and promote the inclusion of individuals with disabilities as equal members of society.
Future Directions
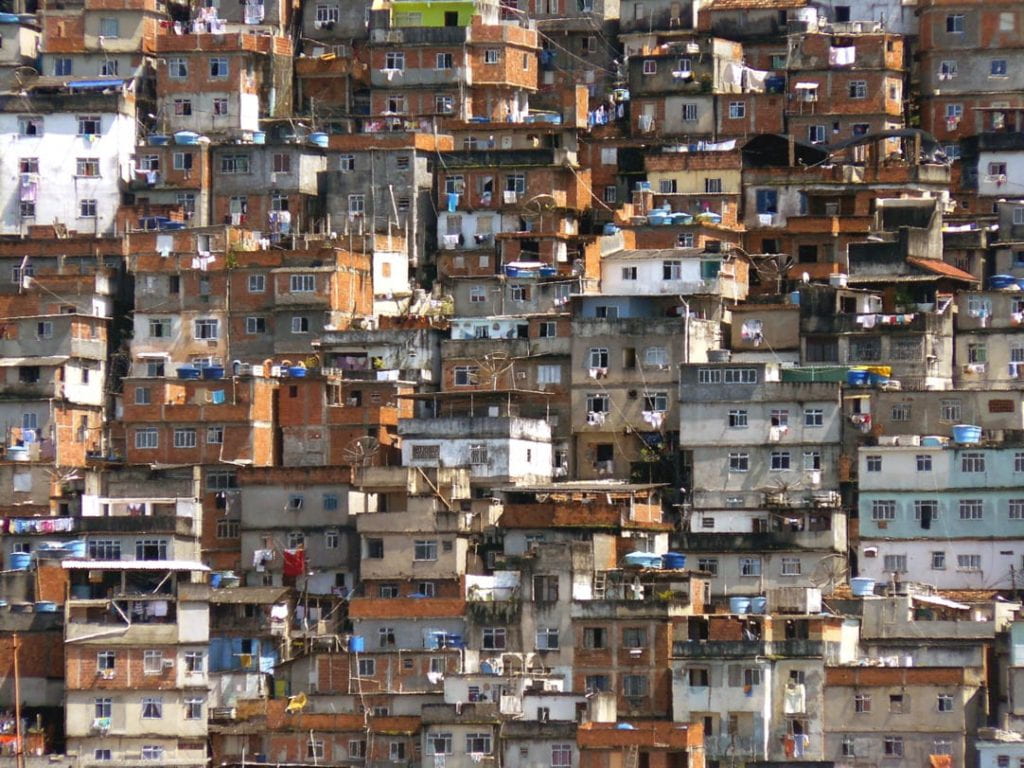
Despite these accomplishments, there is a lot more work that needs to be done. A study by Paul Chaney of Cardiff University revealed that ableism is still pervasive in Indian society. Educational programs for individuals with disabilities are not funded adequately, and private schools often ignore the minimum supports for students with disabilities as required by the law. Individuals with disabilities in rural areas are particularly disadvantaged in terms of educational opportunities, leading to much higher likelihood of unemployment and poverty. Concerns continue regarding the accessibility of the healthcare system for people with disabilities. Still, efforts are being made to combat forced institutionalization and forced sterilization of individuals with disabilities, issues which compound at the intersection of gender discrimination.
The successes discussed in here are just a few examples of the change created by the disability rights movement across the world and the driving force behind it: namely, the advocates who work tirelessly to push society forward in its inclusion of individuals with disabilities. Although more progress is yet to be made, these testimonies give us hope that transformational change can occur, however gradually it may come about. This is our letter of gratitude to those who continue to work to ensure the equitable and rightful treatment of individuals with disabilities and our call to action to all others.