In 1950, the office of the United Nations High Commissioner for Refugees (UNHCR), also known as the UN Refugee Agency, was created to help millions of Europeans who had fled or lost their homes during World War II. Since the creation of the UNHCR, the UN Agency for Refugees still remains the leading UN organization mandated to protect the basic needs and human rights of refugees. The unprecedented forced displacement of people, both internally and across borders, is one of the most persistent manifestations of humanitarian crises and conflict in the modern era. 65.5 million people around the world have been forced from their homes due to violence. Among the 65.6 million people, the UNHCR oversees more than 21 million refugees, over half of whom are under the age of 18. Presently, the rights of refugees are protected by the UN Convention Related to the Status of Refugees adopted in 1951, established from Article 14 of the Universal Declaration of Human Rights (UDHR). Article 14 of the UDHR recognizes the right of persons to seek asylum in other countries from persecution in their home country.
The long- and short-term effects of displacement on the masses of global refugees generate humanitarian crises for these persons. Humanitarian responses to crises focus on delivering equitable and quality public health interventions, an essential element of the larger operational framework of humanitarian aid. Public health encompasses a vast variety of components including: 1) reproductive health, 2) disease control, 3) maternal and child care, 4) psychosocial support, and lastly 5) sanitation. “Although the health needs during and after natural disasters and armed conflicts are similar, the differences arise from the political complexities of the latter, in which civilian populations serve as targets of war and human rights abuses aggravate health and protection needs” (Leaning, 2013). The main health consequences of armed conflicts are not conflict-related injuries and deaths. During humanitarian crises such as armed conflict, death is exacerbated by various direct and indirect factors, including common childhood illnesses such as diarrheal disease and severe malnutrition. The legitimate concerns of public health equity in the framework of refugees’ and internally displaced populations’ (IDPs) healthcare continues to be more complex and challenging.

Urban Refugees
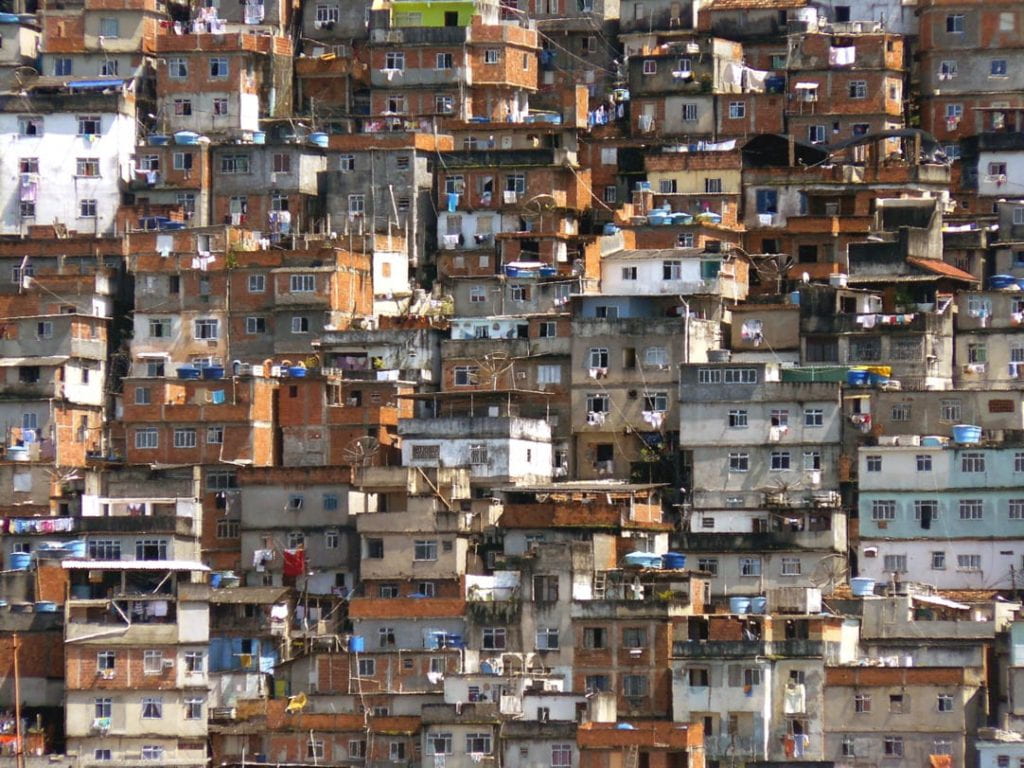
Current global trends indicate a shift towards urban destinations for refugees and away from refugee camps. The UNHCR reports 60% of the global refugee population and 34 million IDP population live in urban environments. Urban environments provide social security for refugees. Unlike refugee camps, living in cities offers refugees the opportunity to live anonymously. Refugees residing in urban settings are not subjected to the limitations of a refugee status and camps. In urban settings, refugees have access to educational, advanced healthcare services, and employment opportunities which may not be available at refugee camps. Examples of this trend are Damascus, Syria and Amman, Jordan; both received more than 1 million refugees from Iraq alone. Furthermore, many refugees are not legally permitted to settle in urban centers, thus end up living in informal settlements and slums alongside the major urban areas. These informal settlements are typically outside the radar of government and humanitarian aid agencies, thus remaining unidentified and particularly at risk for human right violations.
Public health equity in humanitarian situations
From the public health perspective, it is much more difficult to keep track of people when they move to urban areas. This consequently makes healthcare delivery more difficult in terms of: 1) assuring refugees receive basic health care services, 2) coordinating patient referrals, 3) accessible and available health services and resources, and finally 4) managing the costs of health care services. UNHCR’s leading principles for public health assert health care services delivered to refugees by host countries should resemble and correspond with the services provided to citizens and residents in their country of origin. Minimum, yet essential, health care services must be maintained in all situations, including humanitarian disasters and mass forced migration. “This UNHCR guiding principle preserves a sense of fairness and equity between two contiguous groups of people who must, for a range of security and political reasons, be encouraged to live in this adjacency as harmoniously as possible for an indefinite period of time (Leaning, 2011).”
A coordinated system of health care delivery is more urgent in urban settings not associated with refugee camps or humanitarian relief. The urban displacement phenomenon has shifted the direction of care delivery systems to focus on establishing healthcare delivery systems supporting access to preventive health care services. Present systematic healthcare delivery issues requiring critical consideration include 1) the financing of health services, 2) access barriers to services due to unaddressed financial burdens, 3) cultural barriers, and lastly 4) and the integration of services for refugees within existing formal health systems.
Recently, UNHCR has begun to advocate for refugees to gain access to health insurance in their host country, especially in middle-income countries where healthcare systems already function for host populations. For example, in 2011, health insurance for Afghan refugees living in Iran was introduced. By June 2012, 347,000 refugees registered for health insurance. 40% of the Afghan refugees whom enrolled for health insurance were officially registered with the UNHCR. With health insurance, refugees have access to secondary and tertiary healthcare services for treatment of non-communicable diseases and other illnesses. Health insurance provides UNHCR registered refugees a second form of official documentation. Secondary healthcare services include consultant led-services with health care specialists. Tertiary care services include specialized consultative care delivered on referral from primary and secondary The Iranian government also benefits from providing health insurance to the country’s population by reducing the perennial risk of paying for the hospitalization of refugees. Refugee health insurance is successful in Iran because refugees have access to employment allowing some refugees the means to afford to pay premiums and co-payments. The UNHCR will support vulnerable persons if they cannot afford health insurance. Urban refugees need more representation and support services within the health sector.
Resource Allocation
Achieving public health equity in humanitarian crises is a complicated and challenging process. The majority of refugees do not live in refugee camps and their experiences as urban dwellers must be further investigated by academics and professionals alike. This trend holds for human societies in general; the world at large is experiencing rapid urbanization. In 1950, less than 30% of the world’s population lived in cities and towns. Presently, urban population has increased to 54% and is expected to reach 60% by 2030. Even though urban refugees have the ability to live anonymously and earn wages, living in an urban setting undermines refugees’ access to affordable and high-quality basic health care services. Future policy decisions and international aid programs regarding urban refugees must continue to adapt to the shifting demographic profiles of refugees, IDPs and the effects of global urbanization. Ultimately, public health equity problems the humanitarian community is attempting to confront can be categorized under two categories: resource allocation and decision-making. As humanitarian crises stemming from armed conflict become more common, investing in sustainable policy solutions for resource allocation in the health sector for forced migrants will prevent the suffering of these individuals on the low end of the welfare continuum.
