The previous blog posts in this series are located here:
Human Rights in the Appalachian Region of the United States of America: an introduction
Human Rights in Appalachia: The Battle of Blair Mountain and Workers’ Rights as Human Rights
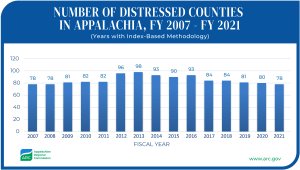
In the Appalachian region of the United States, there have long been overarching socioeconomic problems that have prevented the region from seeing the same levels of growth as other parts of the country, and even been part of its decline in other domains. Much of Appalachia’s population of twenty-five million people remains remote, isolated from urban growth centers and beneficial resources that exist in cities. The rural towns and counties in which many Appalachian people live have not had the ability to maintain the public infrastructure, furnish the business opportunities, or provide the medical services that are necessary to sustain populations.
There are three regions of Appalachia: the southern region, which covers parts of Georgia, Alabama, Mississippi, the Carolinas, and Tennessee; the central region, which covers parts of Kentucky, southern West Virginia, southern and southeastern Ohio, Virginia, and Tennessee; and the northern region, which includes parts of New York, Pennsylvania, northern West Virginia, Maryland, and northern and northeastern Ohio. While the entire Appalachian region struggles with higher levels of poverty, unemployment, and lack of services and infrastructure, some sub-regions suffer worse than others, and in different ways (Tickamyer & Duncan).
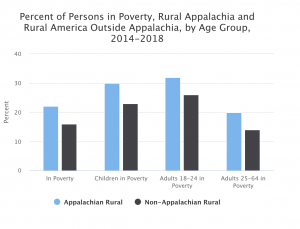
Even when compared to other rural areas, Appalachia struggles on measures of educational attainment, household income, population growth, and labor force participation. Rates of disability and poverty are significantly higher in rural Appalachia than they are in other rural areas of America. In 2018, the number of Appalachian residents living below the poverty line was higher than the national average in every age group except those 65 and older. The largest disparity was among young adults (18-24), where the Appalachian population was more than 3% higher than elsewhere. From 2009 to 2018, median household income in Appalachia went up by 5%, not far behind the national average of 5.3%. However, the median household income in Appalachia remains more than $10,000 lower than the national median.
One area where disparities between Appalachia and elsewhere in the country are particularly noticeable is in healthcare. The Appalachian Regional Commission released in 2017 “Health Disparities in Appalachia”, which reviews forty-one population and public health indicators in a comprehensive overview of the health of the twenty-five million people living in Appalachia. The study found that Appalachia has higher mortality rates than the rest of the nation in seven of the nation’s leading causes of death: heart disease, cancer, COPD, injury, stroke, diabetes, and suicide. In addition, diseases of despair are much more prevalent in Appalachia than the rest of the country. Rates of drug overdose deaths are dramatically higher in the Appalachian region than the rest of the country, especially in the region’s more rural and economically distressed areas. Research indicates that diseases of despair will increase under COVID-19, as well. This will be especially true for women, who experience death from diseases of despair at a rate 45% higher than the national average in Appalachia. The ARC found that, while deaths as a result of diseases of despair were more numerous in metropolitan counties of Appalachia, rates of suicide and liver disease were higher in rural counties.
These issues are exacerbated by the fact that there is a much lower supply of health care professionals per capita, including primary care physicians, mental health providers, specialists, and dentists in Appalachia. The supply of speciality physicians is sixty-five percent lower in the central sub-region of Appalachia than the rest of the nation as a whole. Other factors negatively impact health in Appalachia, as well. Nearly twenty-five percent of adults in Appalachia are smokers, compared to just over sixteen percent of all American adults, and obesity and physical inactivity are extremely prevalent. However, it is worth noting that in some areas of public health interest, such as the occurrence of STIs/STDs and HIV, Appalachia does better than the rest of the country. Healthcare disparities are an increasingly dramatic phenomenon. From 1989-1995, the cancer mortality rate in Appalachia was only 1% higher than the rest of the US, but by 2008-2014, it had risen to be 10% higher. In the same time frames, the infant mortality rate was 4% higher versus 16% higher, respectively. And, in 1995, the household poverty rate in Appalachia was 0.6% higher than the national average, but by 2014 was 1.6% higher. We like to think of these problems as things of the past, but the gaps are still very much relevant. Fortunately, people living in Appalachian communities are more likely to have health insurance coverage than other Americans. 8.8% of the population in Appalachia do not have health insurance versus the national average of 9.4%.
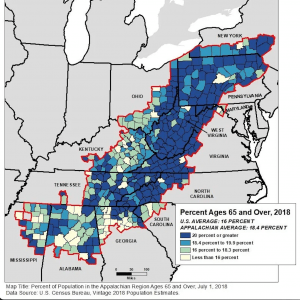
This year, in the midst of the coronavirus pandemic, some factors of the Appalachian population have put people living there at greater risk of COVID-19. 18.4% of people living in Appalachia are over age sixty-five, which is more than two percent higher than the national average. In more than half of Appalachian counties, over 20% of people are older than 65. This, combined with high rates of obesity and smoking, put many people in the “high-risk” category. COVID-19 has affected Appalachian communities in ways that don’t result in death but make surviving even more difficult. Food insecurity, for instance, is an increasingly severe problem. At one soup kitchen, “…we were serving about 200 people a day, and our numbers have nearly tripled since COVID started,” social worker Brooke Parker, from Charleston, West Virginia, said.
However, perhaps due to the isolated nature of many Appalachian communities, mortality rates from COVID-19 have not been markedly higher than the national averages.
With schools moving to online learning, problems with access to internet in Appalachia become more relevant and pressing. Around 84% of Appalachian households have a computer, which is five percentage points below the national average. 75% have access to reliable internet, which is also five percent lower than average. There is no easy solution to this lack of access to education. Even in non-Appalachian counties, students are being severely impacted by the disruption to their normal education activities.
Human rights organizations ought to keep a close eye on Appalachia as we see the results of COVID-19 on an already vulnerable and at-risk population. The ultimate consequences of the pandemic will likely be more severe here than elsewhere in the country. People living in Appalachia deserve the same assistance being offered to and resources being put towards urban centers in other parts of America. Too often have they seemingly been forgotten.
Additional References:
1. “Health Disparities in Appalachia”. Marshall, J.,Thomas, L., Lane, N., Holmes, G., Arcury, T., Randolph, R., Silberman, P., Holding, W., Villamil, L., Thomas, S., Lane, M., Latus, J., Rodgers, J., and Ivey, K. August 23, 2017. https://www.arc.gov/wp-content/uploads/2020/06/Health_Disparities_in_Appalachia_August_2017.pdf. Retrieved December 3, 2020.
2. Population Reference Bureau. https://www.prb.org/appalachias-current-strengths-and-vulnerabilities/. Retrieved December 9, 2020.
3. Tickamyer, A., Duncan, C. (1990). Poverty and Opportunity Structure in Rural America. Annual Review of Sociology. 16:67-86.