by Marie Miguel

Some people believe that PTSD is only a mental health condition that affects those who have come back from war, but this isn’t the case. People who have Post Traumatic Stress Disorder aren’t just veterans. Individuals with PTSD have experienced severe trauma. It’s not only people that come back from combat, but that’s how many of us associate the disorder. PTSD can happen to anybody who experiences trauma such as a sexual assault, a natural disaster, or many things that would prompt someone to have a traumatic reaction, so let’s stop talking about PTSD as though it’s something that only war veterans experience. Anyone who has been through a traumatic experience can develop PTSD. According to the National Alliance on Mental Illness (NAMI), PTSD affects 3.5% of the U.S. adult population. That works out to eight million American people living with the condition. Approximately 37% of people diagnosed with PTSD display serious symptoms. Women have higher rates than men. Later in this article, we’ll discuss the gender divide.
What is Post Traumatic Stress Syndrome?
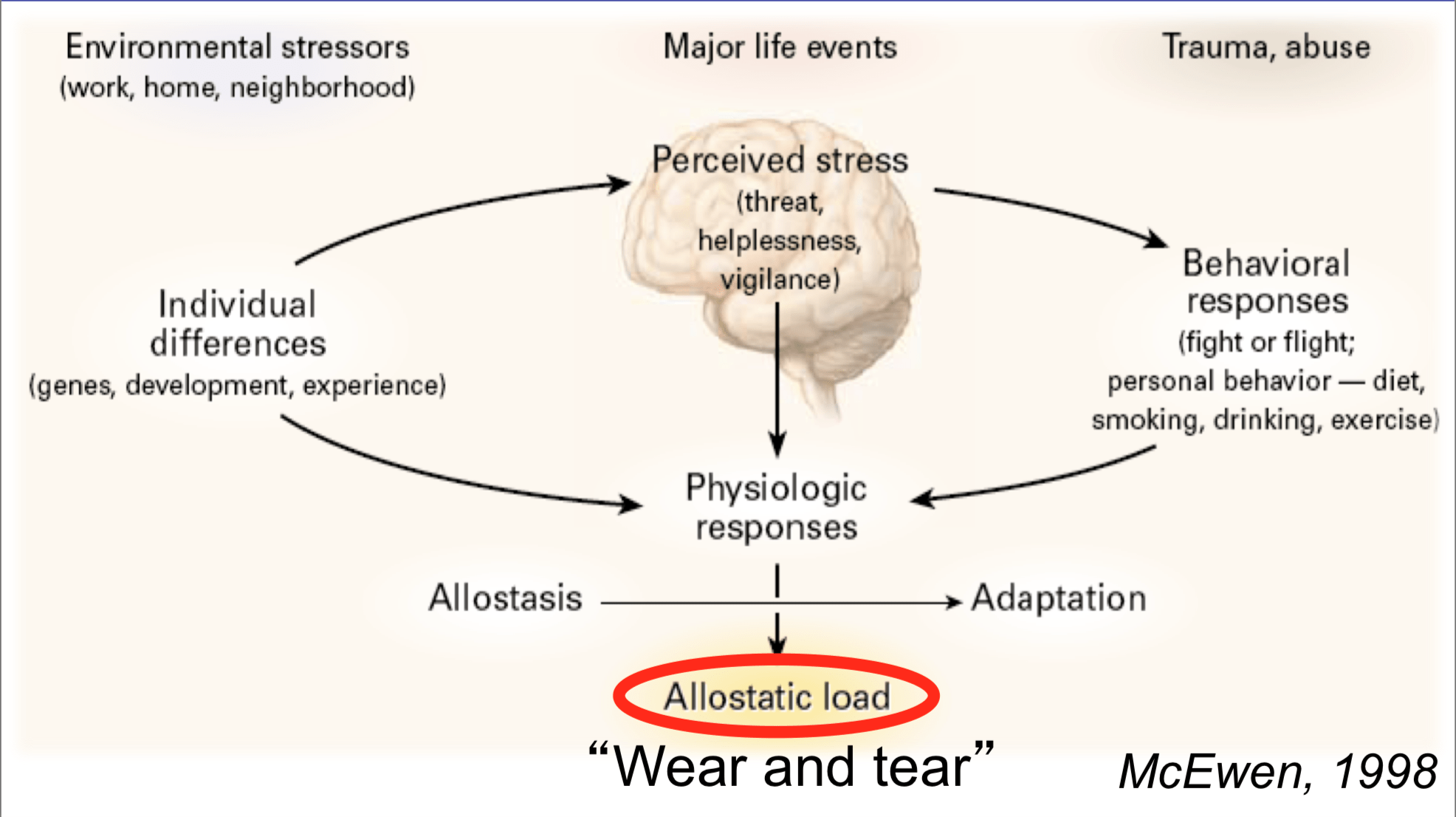
Post Traumatic Stress Syndrome happens after a person experiences trauma, and it’s something that sticks with a person. Symptoms can include flashbacks, night sweats, insomnia, panic attacks, and isolating from friends and family. We need to understand that people with PTSD aren’t dramatic; they’re traumatized. When you experience trauma first-hand it changes your brain. According to the U.S. National Library of Medicine – National Institutes of Health, Several areas of the brain are involved when a person experiences PTSD. A stress response includes the amygdala, hippocampus, as well as the prefrontal cortex. PTSD and trauma can cause lasting changes in those areas of the brain.
What causes PTSD?
The cause of PTSD is that a person experiences trauma and never adequately deals with the issues because it sticks with them. People think that PTSD is caused by being in combat because combat can be a traumatic experience, especially if you see someone die in front of you. The cause of PTSD is when an individual has difficulty adjusting after a traumatic event; their brain changes and the memory of the traumatic event gets stuck in their brain. These intrusive memories make it difficult for an individual to function. The root cause of PTSD is a traumatic event, but the symptoms are what overwhelm people to the point where it’s diagnosable. People with PTSD often have recurring distressing and upsetting memories of the trauma, and when you continually have upsetting memories and can’t stop them, it makes you want to shut down, which is a problem that many people face when living with PTSD, and it can seriously impact your relationships.
Causes of PTSD
- A stressful experience
- Trauma
- Mental Illness
- Predisposition to mental illness or family history of mental illness
Risk factors for PTSD:
- Long lasting trauma
- Childhood sexual abuse
- Other childhood trauma
- A job where you’re exposed to trauma such as a military position
- If you don’t have a sound support system
- Seeing someone get hurt
- A history of substance abuse
Types of trauma
When we think of PTSD, we might think of combat, but it’s not just that. Anyone who has experienced trauma is at risk of developing PTSD. Whether you witnessed a violent act or you were physically attacked yourself, you’re at risk for PTSD. In addition to combat, types of trauma that can induce PTSD include but aren’t limited to:
- Childhood sexual abuse
- Other childhood trauma
- Sexual assault or violence
- Physical assault
- Natural disaster
- Being attacked with a weapon
Symptoms of PTSD
Symptoms of PTSD can range from mood symptoms to physical symptoms. These symptoms can include but aren’t limited to nightmares, irritability, being easily startled or frightened, trouble sleeping or concentrating, or even feeling completely emotionally numb. These symptoms occur after a traumatic event and are only some of the possible signs that an individual could experience. Everyone reacts to trauma differently. And it’s understandable that someone may shut down, lash out, or break down crying. These are all responses that could happen.
How intense are your symptoms?
Depending on the person, the intensity and type of PTSD symptoms will differ. If you have suicidal thoughts or ideation, it’s incredibly crucial to reach out to a friend, loved one, or to contact the national suicide prevention hotline (1-800-273-8255 or 1-800-273-TALK in the United States.) It’s essential that you talk to your doctor if you’re experiencing difficulty functioning.
Complications of PTSD
PTSD can impair someone’s function to the point where they’re unable to engage in normal life activities. Someone might develop substance abuse issues, an eating disorder, or other comorbid mental health conditions. PTSD can be debilitating. It can lead people into a state where they can’t work. It can make it so that they’re unable to attend social functions, and it can severely impact a person’s life. If you’re diagnosed with PTSD, you need to have the following symptoms:
One avoidance symptom – Avoidance is where you’ll stay away from things that remind you of the trauma. Avoidance symptoms include avoiding places and situations that remind you of the trauma, and avoiding thinking about upsetting thoughts connected to the event
At least two arousal symptoms– Arousal symptoms of PTSD make a person extremely anxious. Arousal symptoms include:
- Getting startled easily
- Feeling tense
- Having problems sleeping
- Angry outbursts
At least two cognition/mood symptoms – Cognitive symptoms of PTSD can rob people of things they once enjoyed. Cognitive symptoms include difficulty remembering the trauma, distorted emotions including guilt, and loss of interest things you once enjoyed
One re-experiencing symptom – Re-experiencing a key marker of PTSD, and it sounds exactly like what it is; re-experiencing. Re-experiencing symptoms include flashbacks or reliving the trauma, nightmares, or scary thoughts.

Children vs. Adults With PTSD
Children can have different responses to trauma in comparison to adults. They might wet the bed or have selective mutism, they might start acting out during play time, or they might begin experiencing separation anxiety. According to the National PTSD center, seven or eight out of every 100 people experience PTSD at some point during their life. Not every person who has PTSD has been through a dangerous incident; some people experience it after a loved one has suffered harm.
According to The U.S Department of Veteran Affairs Studies, approximately 15% to 43% of girls and 14% to 43% of boys experience significant trauma. Of the children and teens that experience trauma, 3% to 15% of girls and 1% to 6% of boys go on to develop Post Traumatic Stress Syndrome.
We can see that females seem to develop PTSD more than men do. What is the reason for this? Many women are survivors are sexual assault, try to speak up and aren’t believed. According to the National Sexual Assault Resource Center, one in five women and one in 71 men will be raped at any given point during their lives. Yet, we as a society do not believe survivors as we should. We need to start believing women when they come forward. When we do they can get treated for what happened to them appropriately.
Why do some people get PTSD and others don’t?
You may be wondering why some people develop PTSD while others do not. Part of it has to do with having the risk factors listed above, but there’s nothing wrong with you if you have PTSD and someone else in the same situation did not. There are other disorders that can go along with PTSD. An individual with PTSD can have additional mental health conditions. They may also struggle with suicidal ideation and may attempt to take their life. Here are some mental health conditions that people with PTSD also manage:
- Generalized Anxiety Disorder
- OCD
- Depression
- Borderline Personality Disorder
- Substance Abuse
How to prevent PTSD
PTSD isn’t necessarily preventable because you can’t control when trauma happens, but you can deal with the trauma after it happens. After experiencing a traumatic event, it’s vital to seek mental health treatment in the form of therapy and, if you need to, a psychiatrist. You can reach out to people in your network and find someone to treat your symptoms. Whether you see someone online or in your local area, PTSD is treatable and even preventable if you address trauma right away. If you develop PTSD, it’s okay, and there’s no need to feel shame. It’s a treatable mental illness, and you’re not alone. Many people live with PTSD, and with support, you will get through this. It starts with getting help from a mental health professional, whether that’s working with someone in your local area or finding the help of an online counselor, like one at BetterHelp, you can find a treatment plan and get the help that you need to health from PTSD. You’re not alone, and remember that millions of Americans live with the condition. By going to therapy, you’re doing something incredibly brave, which is taking charge of your mental health. You will get better, but it’s going to take time. Be patient with yourself. Healing from trauma can be difficult, but it’s worth it.
Marie Miguel has been a writing and research expert for nearly a decade, covering a variety of health-related topics. Currently, she is contributing to the expansion and growth of a free online mental health resource with BetterHelp.com. With an interest and dedication to addressing stigmas associated with mental health, she continues to specifically target subjects related to anxiety and depression.