Last Thursday, Dr. Harriet Washington conducted a seminar with the UAB Institute for Human Rights where she discussed the contents of her book, Medical Apartheid. Dr. Washington has been the recipient of the American Library Association Black Caucus Non-Fiction Award and currently teaches bioethics at Columbia University. The seminar was moderated by Dr. Kecia Thomas, the Dean of UAB’s College of Arts and Sciences.
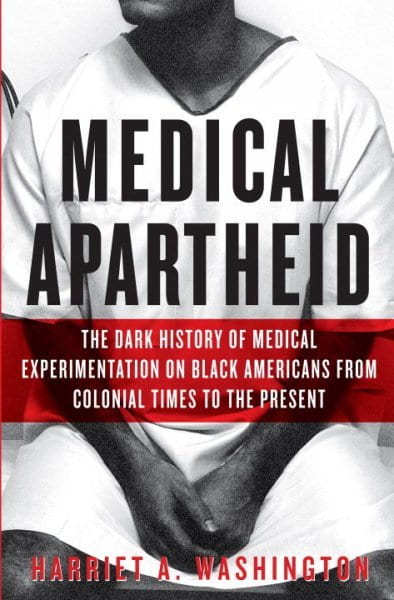
In the discussion, Dr. Washington highlighted several aspects of medical treatment of black people that previously went unnoticed. Her motivation for her highly popular book, Medical Apartheid, was a file she discovered in the 1980s during her job at a hospital. At that time, talking about diversity was a taboo thing. But as she was working one day, she came across an old filing cabinet with patient files from the 1970s of people who needed kidneys. As she began sifting through the files, Dr. Washington analyzed the social profiles of those patients and observed a key difference — the files of ethnically white people were much thinner than that of black people. That was a precursor to her next discovery–one of the files of a black person had the word “Negro” underlined, and the health plan laid out was that of imminent demise, not for healthcare. In that moment, Dr. Washington grew acutely aware of racial plights within the healthcare system and of the inferior care that was being offered to marginalized communities.
In 2001, she was invited to an international conference on human medicine in Germany, where the only discussion of the mistreatment of African Americans in medicine was the Tuskegee crisis. This claim was boldly made by the international community because there were no other major records of such mistreatment in healthcare. In that moment, Dr. Washington decided to write Medical Apartheid “so no one can decline this ever happened in history.”
Why use “apartheid”?
According to Dr. Washington, that is precisely what her discovery is. Dr. Harold Freeman, a cancer surgeon in New York, found in 1990 that the men of Harlem, NY had medical profiles similar to the men of Bangladesh. Such a finding is shocking and very disturbing, but Ms. Washington described internalizing his information as an indication of a foundation that enables such actions to be discoverable. The reason why these medical disparities translate to an apartheid is because we have highly effective historical policies that have and continue to succeed in making us “two different Americas.”
While this history and factual information has been ignored for too long, people seem receptive to this information and have been utilizing the history in an attempt to correct it. That is why calling the movement what it is — an apartheid — and doing everything in one’s power, be it from the capacity of an educator or a student, use the information to actually influence a change.
Vaccine Hesitancy
Dr. Thomas shifted the focus of the conversation towards the COVID-19 pandemic and the speculations of vaccine hesitancy among black people being a consequence of the Tuskegee Scandal, an event where black people were given a placebo of the cure for syphilis. This myth, however, was quickly busted by Dr. Washington who first stated blatantly that the American healthcare system is untrustworthy, so blaming people for being untrustworthy of it is unfair to do. She continued to quote a study that founded that black people who have never heard of the Tuskegee scandal are more scared of vaccines than those who are familiar with the medical injustice; thus blaming Tuskegee, according to Dr. Washington, is a form of laziness. Rather than speculate on behalf of black people, and people of color (POC) in general, Dr. Washington’s suggestion is to ask and clarify why POC are less likely to participate in clinical trials. Her own research indicates that prioritizing an elderly age group in such trials is synonymous to penalizing POC, for POC tend to be younger populations while white people have a larger older population. The solution to this is creating more nuanced policies that take into consideration restrictions like not having insurance or limited internet access.

Ethics and Informed Consent
Another area of medicine Dr. Washington specializes in is the ethics of clinical trials and the common violations of informed consent that researchers often engage in. Fraud and deceiving POC in trials is not a new concept; it happened in the Tuskegee trials and continues to happen, unfortunately. In 2006, only black people were given artificial blood to see if they would still heal from the disease treatment being tested; the subjects died of heart attacks because of this deception. While we know placebos exist in clinical trials, administering the placebo to a select group of people rather than across the tested subjects, irrespective of race, is something which is unethical and illegal.
Actions to Take
First, we must be willing to eradicate our generations of ignorance towards people of color, especially black populations, starting with valuing their lives. Having open conversations such as the one had with Dr. Washington is a great place to start because the only thing that is being presented is facts and evidence corroborating a painful yet honest history of medical apartheid. And implementing the information we learn in our research and education is one step we can all take to put an end to this apartheid. The second thing anyone can do is openly advocate for nuanced policies that are socially and economically aware of the implications and disadvantages current policies present to diverse populations. Urging our public servants to pay attention and take action against healthcare injustices is yet another change we can bring forward amid the pandemic, a time that has taught our global community the immense need for a united front against injustices.
