While experiencing record high heat in NOLA, we navigated the busy streets to City Hall, where the New Orleans Department of Health (NOHD) is located. We made our way through security to the 8th floor, overlooking the city that is known for its vibrant culture, jazz musicians, and amazing food.
“Hello, everyone! Welcome!” exclaimed Monica Hernandez-Wilmer, Special Assistant to the New Orleans Health Director, while we stood in the dim, marble-lined hallway. Greeted with smiles and open arms, we all felt welcomed and at home when we were introduced to everyone. Fran Lawless, the NOHD Health Director, greeted us and explained to us the mission and vision that they refer to when they are protecting the health of the residents of The Big Easy.
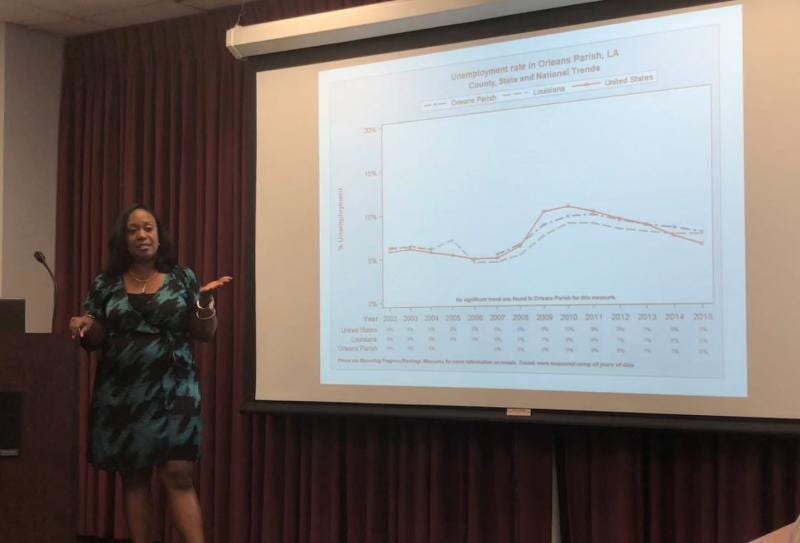
After getting settled in, Katherine Cain, the Quality Improvement & Performance Management Program Leader, led a presentation that described the city, its demographics and health statistics. She discussed the numerous programs that the department has incorporated. The goal? To improve the health and well-being of all of its citizens.
We found that the NOHD is very much aware of the many health disparities throughout the city, and they are doing everything that they can to eliminate them with the limited funding they’re given. They are partnering far and wide with entities such as the LA state health department, the LA Public Health Institute and many non-profits throughout the city (such as Our Daughters of Charity, which is next up on our tour) to provide the needed services and programs that the health department doesn’t have the funding to do alone. They are applying for grants and looking for other sources of funding to supplement the federal pass through dollars they receive from the state and the limited budget they receive from the city (0.3% of the city’s total budget goes to public health.) They are walking the tightrope between prevention and treatment on a rope made of limited funding.
The mission of the New Orleans Health Department is to protect, promote, and improve the health of all where we live, learn, work and play. This is seen through the programs and services that they have available for the public. The two programs that seem to enhance and protect the culture of the city are the smoke-free ordinance and the soundproof initiative. Within the smoke-free legislation, restrictions are placed on where people are able to smoke cigarettes (regular and e-cigarettes) and vapes. Whereas, the sound proof initiative is to protect the community from loud noises through education (exposure and length) and hearing protective devices. According to Cain, these ordinances allow for the protection of not only the public, but of the musicians who keep the music flowing and the culture alive. Another important program is Healthcare for the Homeless. This allows for men and women, regardless of health insurance status, to receive primary health care services.
Included in the care are the following:
* Annual check-ups
* Immunizations
* STD and HIV testing
* Dental Services
* Medicaid Sign-up
* Behavioral Assessment
Without the expansion of Medicaid in New Orleans, certain programs would not have been accessible or even possible. This expansion led to health insurance coverage to be widely spread throughout the state, especially dental care and mental health services. To improve on the mental health care status of the city, the New Orleans Health Department has a partnership with NOLA police. Within this collaboration, the officers are trained to identify and communicate effectively with persons with suspected mental health issues. Not only are the police trained in sensitivity, but they are able to refer the people to case managers and get them the care and treatment they need.
It is the citizens of New Orleans that make this city thrive, so it is vital that they are healthy no matter their socio-economic status. Torrie Harris, DrPH, MPH, the NOHD’s Health and Equity Strategist, stated the importance of health in all policies, and ensuring that those policies are equitable for everyone in the city. As the department continues to support the community efforts that fill the voids left in the city, they continue to launch additional efforts to achieve health equity. It is without a doubt that New Orleans is the heart of Louisiana, and even in sweltering heat there is no place like NOLA.
https://www.nola.gov/health-department/
Team #3 — Alyse, Danielle, & Deanne